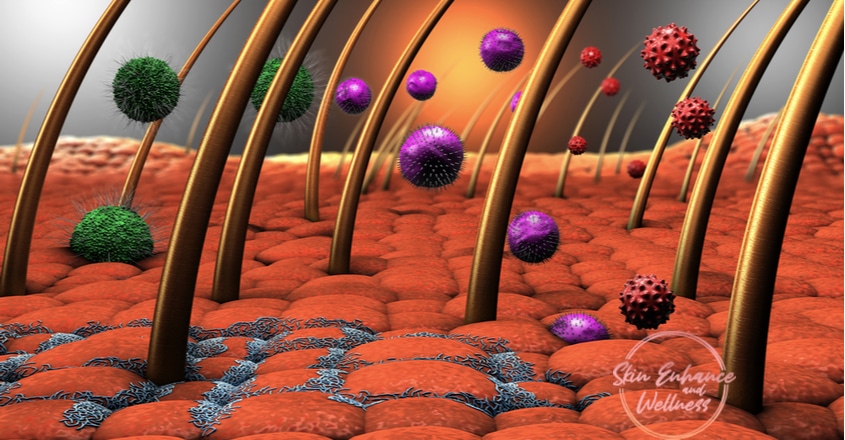
We have a whole spectrum of microorganisms that live on our skin that either exists in harmony or even offers protection. We call this the microbiome and includes bacteria, fungi, viruses and mites. The microorganisms that live in harmony with the body are called commensals. They protect us from infection by maintaining the correct condition for our skin to thrive while discouraging unfavourable organisms. The vast majority of commensals are bacteria with fungi being the next commonest. The role of commensal viruses is not known due to the lack of means to study viruses. Mites are more present in some part of the body with favourable conditions.
The skin also has a role as an immunological barrier. It is thought the microorganisms ‘teach’ the skin how to identify danger. Our skin is primmed to regard similar surface patterns on bacteria as a friend or foe and respond accordingly.
When do you get these microorganisms on your skin?
Your body is sterile in the womb and becomes ‘colonised’ within minutes of being born. The microbiome changes as babies grow due to what they are exposed to in the environment. At puberty, due to the hormonal changes, different microorganisms begin to inhabit different areas of your skin. There is a gender variation in the microbiome between males and females. Your microbiome is affected by the environment you live in. Your clothing, cosmetic use, soap use all affect the state of your skin which in turn affect your microbiome. Recurrent antibiotic use has been associated with resistance as well as an imbalance of commensals within the body. A combination of all the above factors makes you unique in what microbiome you possess as an individual.
On your body, moist skin surfaces have a different set of microorganisms compared to relatively dry surfaces. Areas with high hair and sebaceous gland activity affect the organisms able to thrive in this environment.
Microorganism related skin conditions
There are many ways your skin could get infected. For a disease process to occur, there must be an imbalance leading to an overgrowth of a commensal organism already sharing our skin or an invasion by a pathogenic or harmful organism.
This can be influenced by:
- Age of the host- If you are very young or very old.
- Immune system- If you have a compromised immune system due to an autoimmune condition, immune suppression medication or Human Immunodeficiency Virus infection (HIV)
- Breach in the physical skin barrier by an ulcer, surgery, other infections, etc or presence of foreign body such as an indwelling catheter, heart valves, etc in your body.
You are more susceptible to infection if the above applies to you.
In the immunocompromised and the elderly, the commensal may not cause the initial insult but it may cause secondary infections, prevent or even delay healing. In conditions like eczema and psoriasis, due to the breakdown of the skin barrier, commensals can cause secondary opportunistic infections.
Skin disorders associated with microorganisms sharing your skin
There are some skin disorders which are associated with microorganisms you share your skin with. This does not mean an infection, rather an association with the microorganism.
Here are some common examples:
Acne
In acne, there is an inflammatory reaction within the sebaceous glands related to hormonal influence. The bacteria, Propionibacterium acnes (P.acnes) is the most common commensal found in skin rich in sebaceous glands. The inflammatory process in acne allows the proliferation of this harmless commensal. The combination of increased bacteria level and the presence of inflammation leads to the development of pustules and nodules in the skin.
Acne: The unexpected, uninvited, unwanted pain in the face!
Rosacea
The Demodex mite is thought to release bacteria on its death on to the skin surface and this is thought to set off an inflammatory reaction. Although present in all humans, people with rosacea are thought to have a higher than average population of this mite on their skin.
Could the sensitivity on your face be Rosacea?
Seborrhoeic Dermatitis
This chronic scaly inflammatory condition affecting the scalp and face is a type of eczema. It is thought to be caused by an overgrowth of the fungus Malassezia spp.
Skin Infections associated with organisms you are already sharing your skin with
There are some infections that are due to an invasion of our own microbiome or a different organism.
Thrush infections
Yeast is an example of an organism we share our skin with that can overgrow. When there is an overgrowth in the external genital tract, you can experience unpleasant symptoms. This can occur in the presence of pH changes in the environment from soap use or by the use of antibiotics by the host.
Treatment is with topical or local antifungals.
Pityriasis Versicolor
This is a chronic condition causing pigmentary changes on the trunk and it is caused by a yeast that normally shares our skin.
Treatment is with topical antifungals as creams or shampoos.
Impetigo
This is a superficial skin infection caused by the bacteria staphylococcal spp. The bacteria can be introduced by any small scratch that breaks the intact skin barrier. Once present, it is very contagious can easily spread from one part of the body to another or from one host to another.
Although most respond to topical or oral antibiotics, severe infections may need hospital admission for intravenous antibiotics.
Cellulitis
Cellulitis is an acute skin infection caused by bacteria: Streptococcus pyrogens are bacteria we share in the throat or nose in some individuals and Staphylococcus aureus is present on the skin surface. In order to cause an infection, the bacteria have to be introduced into the dermis layer of the skin. Once the infection starts, it can spread rapidly by local invasion. But it is not contagious.
Cellulitis needs to be treated with oral antibiotics and may become recurrent in the same individual. A more serious variant of cellulitis is Necrotising Fasciitis also called ‘flesh-eating bacteria’ which needs surgical debridement and systemic antibiotics as soon as possible.
MRSA (methicillin-resistant Staphylococcus aureus)
This is not a condition, rather a status. As the name suggests, those with MRSA are colonised by bacteria that are resistant to most antibiotics but it can be a harmless commensal in some people in the community. In generally fit and well individuals, we do not test for this or take any action in General Practice. It is only relevant if they need to go into hospital for a surgical procedure where they will be routinely screened for and treated to eradicate it. Being compromised by another disease can also make them more susceptible to contract it.
You are not alone. Bacteria are by far the numerous but fungi and other organisms also share your skin. You can get a local or systemic infection by a pathogen but it is beyond the scope of this blog to discuss all the pathogens faced by the human body hence only a few were discussed.
Despite being exposed to many microorganisms, your skin can discriminate between harmless commensal organisms and disease-causing pathogens prioritising your protection at all times.
If you suffer from Acne or Rosacea and wish to discuss your concerns further, please find below details of how to book your consultation.
📱07825 999 144 or
☎️ 01277 549 006
💌 drtash@skinenhanceclinic.com
Website: Book an appointment

Recent Comments